
Clinical Leaders Playbook for HCC V28 and RADVWebinar Transcript - Hosted by VBC Exhibit Hall and Connective HealthWatch the webinar in its entirety, here.
Introduction
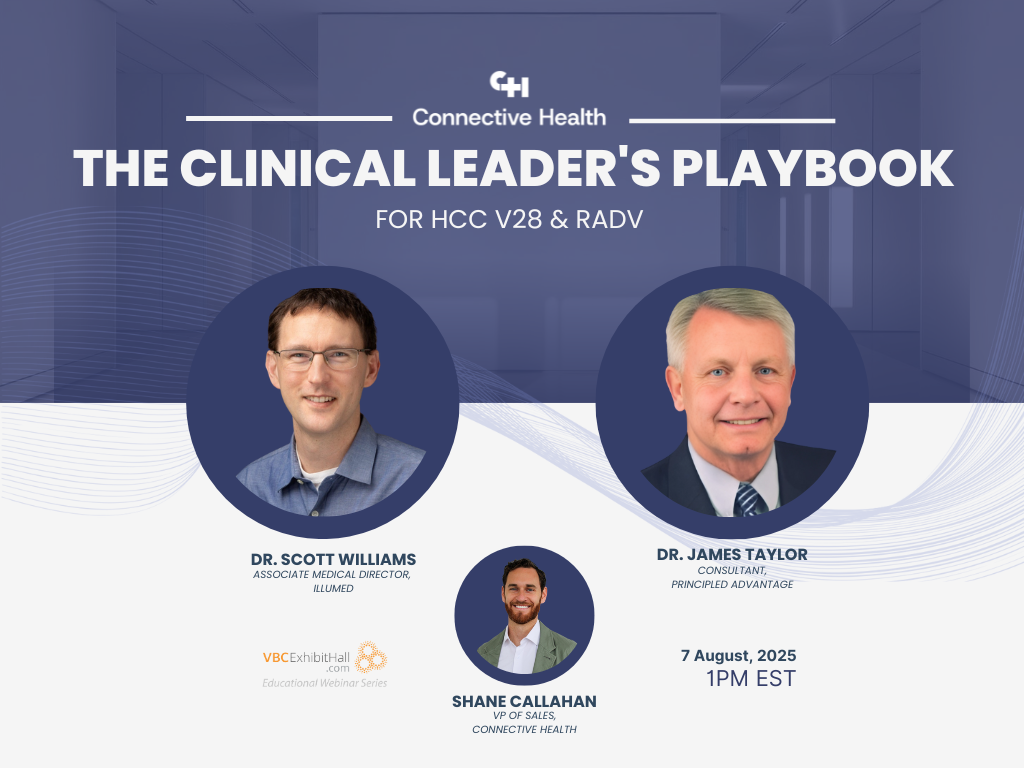
Garrett Schmitt (CEO, VBC Exhibit Hall): Welcome everyone to today's live webinar hosted by Connective Health. This is our first collaboration with them, and I'm excited about today's topic: "The Clinical Leaders Playbook for HCC V28 and RADV."
A few housekeeping items:
- Everyone has joined in listen-only mode
- Submit questions using your attendee module - we'll address as many as possible
- The session is being recorded and will be available with slides via email within an hour
Speaker Introductions
Shane Callahan (VP of Sales, Connective Health): I'll be moderating today's discussion. Connective Health specializes in helping value-based care organizations succeed with actionable external insights - specifically medical records that exist outside of claims data and native EHRs. This enables providers to better engage patients and optimize risk adjustment, quality performance, and utilization management.
Dr. Scott Williams (Associate Medical Director, Illummed): I'm a family physician based in Maine and associate medical director with Illummed, an ACO REACH program based in Florida working with partner groups nationwide. My primary focus is on risk adjustment or "burden of illness" programs. I previously held similar roles at Maine Health and their ACO for Medicare Advantage programs including MSSP.
Dr. Jim Taylor (Former Chair, Colorado Kaiser Permanente Medical Group): I'm a family practitioner with 35+ years of experience and a certified coder for 15 years. I started in small-town Ohio with eight years of private practice, then joined Kaiser for 20 years, with the last 10 primarily focused on Medicare Advantage. I helped Kaiser prepare for Medicare Advantage in 2003 and managed 100,000 Medicare Advantage patients. After Kaiser, I helped start Iora Health's Medicare Advantage line, which was eventually acquired by Amazon. I also served as Humana's national director of Medicare Advantage for one year. My passion is making the right thing to do the easy thing to do while keeping administrative tasks off physicians' backs.
Setting the Stage
Shane: We're here because of the rapidly evolving state of value-based care, particularly the transition to the V28 model and increased rigor of RADV audits. These represent key challenges for ACOs and providers. The increased coding complexity, while clinically useful, is projected to decrease overall risk scores by 3-5% and increase audit frequency, opening providers to more risk.
Our discussion will focus on four key themes:
- How to earn provider attention and enable accurate condition capture without adding to workload
- How external medical records sourced beyond claims are a strategic imperative
- Making chronic condition insights more actionable for providers
- The future of risk adjustment and chronic condition management
Poll Results Summary
Poll 1: Primary Areas of Concern
- 63% - Ensuring accurate and complete clinical documentation
- 17% - Provider engagement and reducing administrative burden
- 15% - Financial impact of potential reimbursement changes
- 5% - Integrating and making sense of data across multiple sources
Poll 2: Biggest Barriers to Consistent Condition Capture
- 52% - Time and competing priorities during patient encounters
- 25% - Understanding how work impacts reimbursement and patient care
- 23% - Training on specific coding and documentation requirements
Poll 3: External Medical Records Usage
- 42% - Have systematic proactive process to ingest and analyze external data
- 26% - Use external data reactively on case-by-case basis
- 21% - Do not currently use external data
- 11% - In planning/exploration phase
Key Discussion Points
The Challenge of Provider Engagement
Dr. Taylor: The biggest clinical barrier is time. We need to make the right thing to do the easy thing to do by turning on certain EMR functions. Change feels better when it's done with you rather than to you, so involving clinicians in the process helps overcome barriers. The focus has shifted from just getting any diagnosis through audit systems to specificity and accurately representing conditions.
Dr. Williams: This transition requires a different mindset. In fee-for-service, you're asked "how much did you do?" - labs, consults, procedures. In value-based care, you're asked "what did you manage?" - the complexity and burden of illness. Systems aren't set up for this; they're designed for fee-for-service efficiency, not necessarily for the most accurate or specific diagnosis capture.
Real-World Example: The Power of Comprehensive Assessment
Dr. Williams: I recall a chart review of a 75-80 year old patient who saw her PCP once yearly with stable asthma and high blood pressure. When I dug deeper:
- Her eGFR had slowly declined over 5-6 years to borderline CKD 3A/3B
- Spirometry showed COPD, not asthma
- She had slow, insidious weight loss becoming borderline underweight
Each condition alone seemed minor, but together they painted a picture of someone in slow decline. When the provider saw this comprehensive view, instead of a routine "I'm doing fine" visit, they had a proactive conversation about goals of care and planning for the next 3-5 years.
Practical Implementation Strategies
Dr. Taylor: Use the "5 seconds now or 5 minutes later" principle. Set up your EMR prescriptions to include the indication (e.g., "hydrochlorothiazide for hypertension"). This propagates every time you reference those medications and provides RADV auditors evidence of active treatment.
Learn the "magic words." We treat hepatitis C, but we mean chronic hepatitis C. If you don't specify "chronic," you'll get a query requiring 5 minutes to answer instead of 5 seconds to document correctly initially.
Focus on getting providers from "wrong" to "okay," not from "wrong" to "ideal." Providers don't want to be perfect; they just want to be compliant and efficient.
The Importance of External Data
Dr. Taylor: Claims data alone is insufficient - I've found 20-30% is incorrect even after auditing. Hospitals code "rule-outs," lab techs input diabetes when drawing blood, oncologists code "breast cancer" when it's actually "history of breast cancer." You need more than claims data and should take claims data with a grain of salt.
Dr. Williams: External data becomes powerful when you can connect claims information with objective clinical evidence. For example, if claims show heart failure, immediately surface the patient's last echocardiogram. This efficiency helps providers validate conditions and guide management decisions.
Future-Proofing Strategies
Comprehensive Chronic Condition Management
Dr. Williams: Risk adjustment is necessary but not sufficient for value-based care success. It's not enough to name conditions; you must manage them effectively. The V28 shift emphasizes clinically meaningful conditions requiring direct, thoughtful, ongoing management. You need data that supports both diagnosis validation and management guidance.
Cost Management Integration
Dr. Taylor: You can outspend any diagnosis capture process. Being aggressive about managing costs while maintaining quality is crucial - and physicians buy into this quickly. Sometimes we'd skip the cheapest test for the most expensive because it was more efficient long-term.
Diagnosis capture flattens out over time - people don't gain new HCCs every year. Focus on patients with increased hospital/ED visits or rising costs to identify new conditions or worsening existing ones.
Key Takeaways
Dr. Taylor: Put something into practice to manage costs. Compared to diagnosis capture, cost reduction is more difficult and requires as much or more attention while maintaining quality.
Dr. Williams: Lead with the clinical aspect. Maintain clear clinical orientation so you know exactly what patients have, then apply evidence-based optimal management. This enables targeted interventions for the right populations and better cost management.
Q&A Highlights
Question: Who is cleaning external data and how do you prevent irrelevant claims?
Answer: No one is automatically cleaning external data - you need help. Automatically ignore single diagnoses from single external sources as they're often wrong. Use systems like Connective Health that link existing documentation to claims and discard unvalidated information.
Question: How do you get providers to engage in chart prep processes?
Answer: Trust is key. Focus on high-impact, well-established diagnoses like heart failure rather than minor conditions. Error on the side of accuracy, not completeness. Gain credibility first with clear, important diagnoses before asking providers to research questionable ones.
This webinar was hosted by VBC Exhibit Hall in partnership with Connective Health.
